Opioid Basics
Opioid withdrawal refers to reducing your usage of opioids until you are able to stop taking the medication completely. You might also hear this referred to as detoxification. Before we get started with your opioid withdrawal options, we’ll cover some basic information.
What are opioids?
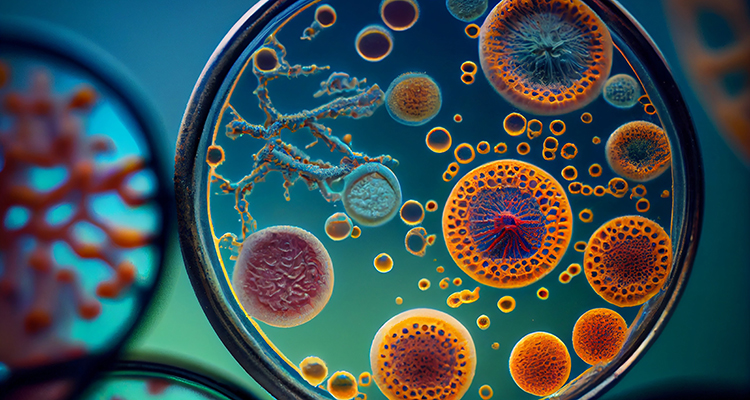
Opioids are very strong painkillers which are commonly prescribed for short term, acute pain, such as recovering from a surgery or when you’ve had a serious injury. In some rare cases where chronic pain is severe, patients may be prescribed opioids in the longer term. This should only happen if all other treatments have been ineffective.
This 2019 article explains that opioids include, “opiates (drugs derived from the opium poppy, including morphine, codeine, heroin, and opium) and synthetic opioids like hydrocodone, oxycodone, and methadone”
We have opioid receptors in specific areas of our body and brain. The body makes its own opioids which attach to these receptors: these natural opioids regulate and reduce pain among other functions. The amount of opioids produced naturally is low, isn’t dangerous, and simply helps our body and mind to function properly. When we introduce medical opioids into our system, they mimic the opioids which naturally occur and attach to the existing opioid receptors to provide pain relief.
Why do people choose to stop taking opioids?
Although opioids can be very effective in providing short term pain relief, in the long term they have many negative effects and risks. Opioids can have many side effects including:
- Nausea
- Drowsiness and fatigue
- Mental ‘fog’ and confusion
- Slowed breathing
- Constipation
- Excess sweating
- Difficulty passing urine
- Itchy skin
- Hormone changes which can affect sexual performance
- Decreased immune function
- Increased risk of fall and fractures
- Dry mouth (often leading to dental problems)
Long term use of opioids can increase the risk of hypoxia, a condition caused by slowed breathing: this results in not enough oxygen reaching the brain. This can have serious long term consequences including, “psychological and neurological effects, including coma, permanent brain damage, or death.”
Over time opioids actually become less effective as your body and mind become accustomed to having them in your system. This means that you need to keep increasing your dose in order to get the same pain relief results you once had. This is a dangerous cycle.
When opioids are taken in the long term it can lead to opioid-induced hyperalgesia, meaning you actually become more sensitive to pain! This study explains that, “The condition is characterized by a paradoxical response whereby a patient receiving opioids for the treatment of pain could actually become more sensitive to certain painful stimuli.”
Opioids are a high risk drug for dependency and addiction. Dependence refers to needing the drug and feeling withdrawal symptoms if you don’t take it. Addiction refers to actively seeking out the drug and misusing the medication. We will use the term ‘relapse’ in regards to both dependence and addiction, which simply means starting to take opioids again after withdrawal.
Why is opioid withdrawal difficult?
When you are taking opioids for a long period of time, your brain and body become used to having them in your system. Your system adjusts to accommodate the additional opioids. Over time the opioids create a sense of wellbeing and even euphoria, which is a welcome side effect for most. A chemical messenger in the brain called dopamine is released in high levels in reaction to opioids. Dopamine creates a ‘reward’ reaction, essentially making the association between an action (taking the opioid) and pleasure (the euphoric feeling).
When you begin to withdraw from these opioids, your brain and body have to readjust to being without them. This can be tough, particularly if you’ve been taking opioids for a long time. During the withdrawal process this sense of euphoria is of course decreased and eventually disappears: in the short term this stark contrast in mood can leave you feeling lethargic, low and depressed.
The side effects of withdrawing from opioids can be significant, and this can be a scary prospect. It’s important to be informed about what might occur during withdrawal, but at the same time this can be off putting. It’s vital to remember that with the right support and an appropriate withdrawal plan, these side effects can be managed. It’s also important to remember why you are choosing to withdraw from your medication and to focus on your end goal.

Even if you are not addicted to your opioids, you can come to depend on them to reduce your pain and to help improve your quality of life. The thought of being without this help can be worrying. You might fear that you’ll be stuck in bed, in lots of pain. You may worry about what the future will hold without this pain relief. No one wants to be in pain, so this is completely understandable! This alone can make opioid withdrawal difficult.
However with the right withdrawal treatment, you should receive support to find other proven, effective methods of chronic pain relief to replace your opioids. You might like to review our detailed post on pain management techniques to understand just how many options are out there for you.
What are the symptoms of opioid withdrawal?
There are a wide range of symptoms which you could experience during opioid withdrawal. Which symptoms are experienced and how severe they are depends on the individual, the type of opioid you were taking, how high your dose was, and how long you’ve been taking the medication. The aim of opioid withdrawal treatment is to try to reduce the side effects you might experience.
Some of the more commonly experienced side effects of withdrawal include:
- Nausea and vomiting
- Stomach cramps
- Muscle and joint pain
- Diarrhea or constipation
- Chills or sweating
- Restlessness, anxiety and irritability
- High emotions and mood disturbances (this can be severe and can include suicidal thoughts)
- Tremors, muscle twitching or other abnormal movements
- Runny nose and watery eyes
- Yawning
- Rapid heart rate
- Changes in blood pressure
- Problems sleeping
- Goosebumps on the skin
- Yawning
- Hallucinations
- Seizures
How long does opioid withdrawal take?
The amount of time it takes to withdraw will depend on many factors, and so will vary for each individual. The dose will be gradually reduced at a rate that suits your individual health needs and circumstances. The withdrawal symptoms are typically at their worst within the first few days, and can last up to two weeks or more.
Risks vs benefits
The risks of withdrawal are of course going through the withdrawal symptoms we’ve discussed. It’s fundamentally not a pleasant experience and can be physically and emotionally taxing. There can also be complications arising from side effects.
The benefits of withdrawing from opioids in the long term tend to greatly outweigh the risks. Benefits of withdrawal include being free from addiction/dependence, being free of opioid side effects, and finding effective ways to treat chronic pain rather than mask it.
Where Do You Start With Getting Help?
Deciding when it’s time
Deciding to withdraw from opioids is a big decision and it can feel worrying. Knowing when it’s time should primarily depend on physical factors such as if you’re experiencing serious side effects which you are struggling to cope with. You might be concerned or have been told by doctors that these side effects have the potential to cause long term damage.
If you are finding that the dose you are taking is not giving you the same relief it once used to, this means that you have built up a tolerance. From then on, you would have to continue increasing your dose to be able to get the same pain relief effects you once had. This is a good indication that it’s time to stop taking opioids.
If you feel you are addicted to your medication or you have been misusing your medication (taking too high of a dose or seeking out medication which has not been prescribed to you), it’s time to reach out for help.
Other factors can play a part in your decision such as feeling that you are at a place in your life where you are ready to explore other chronic pain management options; having enough support around you or access to professional support; and feeling emotionally ready to start the withdrawal process. It’s important to note that it’s rare to feel completely emotionally ready, it’s natural to be nervous and this shouldn’t put you off withdrawing from your medication.
Reaching out for help
It is absolutely vital that when you’re ready to stop your medication, you reach out for help. Do not stop taking opioids suddenly or on your own. This article from Mayo Clinic aptly states, “Don’t try to go cold turkey on your own. Opioid withdrawal can be dangerous, and symptoms can be severe.” This isn’t to scare you, but rather to ensure you get the help you need to start the process safely. Speak to your doctor or specialist about your options. They will help you to taper off your medication safely, with support that is right for you.
Tapering off your medication
Your doctor will put together what is known as an opioid taper schedule, to help you gradually reduce your dose in small increments to make it more manageable. The length of time it takes to taper off your medication completely will vary depending on your individual needs and medical situation. Likewise, the increments your dose is reduced in will depend on the individual. The taper schedule will be detailed, including exactly when and how you should take your medication. It’s vital the tapering schedule is followed exactly.
Care plan
A care plan should be formed with your doctor or health team. This will include assessing your opioid use and your risk of relapse. It should detail which withdrawal treatments are best for you, along with where you should withdraw (outpatient or inpatient for example). The care plan should set out your tapering schedule, what support you will need, how regularly you will be monitored, replacement treatments for your chronic pain, and any additional help you will need going forward.
The plan should account for any additional addiction issues along with any other physical and mental health concerns. The goal of a care plan is to ensure you have the support you need to give you the best chance of success. This should all be discussed fully with your doctor so you understand the choices they are making and the plan set out for you. If you have any questions, be sure to speak up.
Monitoring
When you are tapering off your medication, you need to be monitored to ensure you are safe and to minimize any risks. Monitoring should include:
- Monitoring your vitals to ensure you are safe and handling the withdrawal physically. This might include checking your pulse, temperature, blood pressure and general demeanor.
- Taking urine or blood samples to check the levels of your medication left in your system.
- Talking to you about how you are coping and providing further advice and support.
- Talking to you about your pain level and helping you to manage this as your dose decreases.
- Potentially prescribing other medications to help control withdrawal symptoms and make things more comfortable for you.
- Signposting you to therapy and support options to help you through your withdrawal.
There are a number of ways you may be monitored during the withdrawal process. Which setting is used depends on your own needs, local health service budget and protocols, and how much support you have at home.
Outpatient monitoring
If your withdrawal symptoms are likely to be mild, you don’t have additional health issues and you have good support, it’s likely that you will withdraw from opioids at home. This will involve being in regular contact with your doctor or health team who will monitor you closely. You may visit your doctor regularly for tests, or you may visit a specialized clinic on an outpatient basis.
Going through with the withdrawal process at home can be difficult because you don’t have access to professional help 24 hours a day, and must continue to push forward of your own accord. Temptation can creep up to relapse if withdrawal symptoms become intense. However if you have good support from your loved ones and stick to all of the guidance your doctor provides, it is possible to complete the withdrawal process at home.
Inpatient withdrawal treatment
Inpatient treatment involves staying at a hospital or clinic during the withdrawal process. The staff are trained to help you through the withdrawal process: they will closely monitor you to keep you safe and provide appropriate support. This might involve administering medications to minimize withdrawal symptoms, providing therapy sessions, and assistance with social needs to prepare for discharge.
Inpatient treatment is proven to be more effective for opioid withdrawal, primarily because of the amount of support, constant monitoring, and the avoidance of temptations. However inpatient treatment is typically only used in severe cases or if the patient has other physical or mental illnesses.
Residential treatment
Residential treatment will typically involve going to stay in a house, rehabilitation centre or clinic designed specifically to support those going through opioid withdrawal. You might also hear this referred to as a ‘rehabilitation programme’. You may have your own room or flat, and may be free to come and go (depending on your progress), so it’s more independent than an inpatient setting. However you will still have access to staff 24 hours a day and close monitoring to guide you through the withdrawal process.
Medication-Assisted Treatment
For more severe withdrawal symptoms, medications will be prescribed to help reduce side effects and make withdrawal easier. This report from the National Institute on Drug Use explains that, “Someone in recovery can also use medications that reduce the negative effects of withdrawal and cravings without producing the euphoria that the original drug of abuse caused.”
These medications are typically used in an inpatient setting as they require close monitoring. If they are used in an outpatient setting, regular and very close monitoring would be needed. The dosage for each medication will vary depending on the individual situation.
Clonidine
Clonidine’s original purpose was to treat high blood pressure but in recent years it’s been used to ease withdrawal effects from opioids. It works with specific receptors in the brain to calm the nervous system, which creates a sense of relaxation and pain relief.
Clonidine is one of the most commonly used medications to aid with withdrawal: it can help reduce withdrawal symptoms by 50%-75%. Clonidine can help to reduce anxiety and restlessness, and enable patients to better regulate their emotions, all of which can make the withdrawal experience more manageable. It’s also very effective at reducing cramping, muscle aches, sweating and a runny nose.
Lofexidine
Like Clonidine, Lofexidine’s original purpose was to treat high blood pressure. It can relieve side effects of withdrawal in the same way as Clonidine. Although it’s less commonly used, it can actually be safer for use than Clonidine. This article from Harvard Medical School explains that, “clonidine can cause low blood pressure, which can be a limiting side effect, whereas lofexidine has less of an impact on blood pressure.”
Buprenorphine
Buprenorphine is an opioid replacement. It’s what is known as a partial opioid agonist: it binds to opioid receptors in the brain but doesn’t activate them as strongly as other opioids. It produces less side effects than some other opioids and doesn’t produce the sense of euphoria. It’s often used to make withdrawal more manageable and to shorten the length of time it takes for withdrawal.
Suboxone
Suboxone is a combination of buprenorphine and an opioid blocker called naloxone. The combination does not produce addictive side effects like other opioids. It can aid in reducing withdrawal symptoms and reduce the length of time it takes to withdraw from other higher strength opioids.
Methadone
Methadone is what is known as an opioid agonist: it’s another opioid which binds to the opioid receptors in the brain. It produces less side effects than many other opioids. It’s also much easier to withdraw from as it produces less intense withdrawal symptoms and eliminates the sense of euphoria. Therefore it’s sometimes used in the longer term to help reduce other opioids, before eventually withdrawing from methadone.
Naltrexone
Naltrexone is an opioid antagonist, meaning it blocks the opioid receptors in your brain. This reduces the desire for opioids and can help to make the withdrawal process easier. However it can also block the effects of opioids, so it’s important it’s used correctly in order to prevent withdrawing too quickly and causing more side effects.
Naloxone
Naloxone is a very quick acting opioid antagonist: it quickly gets rid of the effects of opioids within the body and brain. This is only used in the case of opioid overdose when quick withdrawal is needed, as it can produce a lot of side effects and be dangerous if not used appropriately.
Diazepam
Diazepam is a benzodiazepine: it’s a sedative which can help to alleviate withdrawal symptoms such as anxiety, restlessness, distress and problems sleeping. It’s also useful in relieving muscle spasms. Diazepam works by calming the brain and nerve pathways. It is often used during alcohol withdrawal along with other drug withdrawals. Diazepam will only be used short term, as in the long term it can become addictive.
Over The Counter Medications
For mild withdrawal symptoms, over the counter medications may be useful to reduce symptoms and make you feel more comfortable. This is more common if you are withdrawing in an outpatient setting. It’s important to follow guidance from your doctor about what might be suitable for you.
Painkillers
Over the counter painkillers may help to reduce joint and muscle pain which comes as a side effect of withdrawal, along with reducing any chronic pain you might be feeling as you reduce your opioid dose. These might include paracetamol, aspirin and co-codamol.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are also available, which help to reduce inflammation as well as pain. NSAIDS can also be useful in fighting fever, chills and sweating.
Anti-nausea
Anti-nausea medications can reduce both the feeling of nausea to make you more comfortable, and the likelihood of vomiting. These may include medications such as meclizine (Antivert or Bonine) or dimenhydrinate (Dramamine).
Sometimes nausea and vomiting can make you feel like you don’t want to eat or stop you keeping food and drink down, which can make you weak. Taking anti-nausea medication can help you to tackle this.
Anti-diarrhea
Anti-diarrhea medications like loperamide (Imodium) can help to settle your stomach and reduce diarrhea to make you more comfortable. Diarrhea can make you very dehydrated, which can be dangerous, so these medications can be particularly useful.
Antihistamines
Antihistamines may be able to help reduce itching, watery eyes and skin irritation. As well as making withdrawal less distressing, this can increase your chances of being comfortable enough to sleep during withdrawal.
Rapid And Accelerated Detoxification
What is rapid detoxification?
Rapid detoxification refers to withdrawal done under anesthesia, using opioid blocking drugs. This enables doctors to get opioids out of the patient system more quickly. However this method is not used very often, as the risks outweigh the potential benefits.
What are the risks?
Although the opioids may leave the patients system more quickly, the length of time spent experiencing withdrawal effects is not necessarily shortened. Aside from this, the procedure can be dangerous. This article explains that, “vomiting often occurs during withdrawal, and the potential of vomiting under anesthesia greatly increases the risk of death.”
In fact the National Institute for Health & Clinical Excellence (NICE) guidelines which are used to regulate health treatment in England clearly state that, “Ultra-rapid detoxification under general anaesthesia or heavy sedation (where the airway needs to be supported) must not be offered. This is because of the risk of serious adverse events, including death.”
The procedure is typically only offered in exceptional circumstances, or where the individual specifically requests it. In this case, very close monitoring would take place during the procedure to make it as safe as possible.
Non-Pharmaceutical Options
As well as medication assisted withdrawal, there are other options which can help you through with the withdrawal process. The aim of these treatments is to make the withdrawal more manageable and comfortable for you, and to teach you positive coping strategies. This is often known as psychosocial treatment, which can be defined as, “including cognitive and behavioural approaches and contingency management techniques”.
Assistance with social needs
Many people who are struggling with opioid addiction may find it hard to engage with ‘normal’ daily life. Chronic pain itself can be a barrier enough to daily functioning, but when you combine that with dependence on opioids, things can get really tough. A vital part of opioid withdrawal treatment should be assistance with social needs to help patients regain their quality of life and access the support they need.
Employment
Many people with chronic pain and opioid dependency are out of work or struggle to keep up with the demands of a job. Help to get back to work can include providing hope for the patient about other effective chronic pain treatments to enable them to increase their levels of functioning, as well as vocational training. Vocational training centers around educational and training programmes to help you find work and be realistically able to maintain your job. This can include, “skills training, sheltered work environments and monitoring of drug use during employment.”
Housing
Whether an individual is homeless, not in appropriate housing, or in a housing situation which is detrimental to their physical and mental wellbeing, housing assistance services can be useful. This may involve finding temporary accommodation, assisting you with getting the right benefits and financial help if you’re out of work, and finding more permanent accommodation which meets your needs. Being in the right environment is vital to manage opioid withdrawal, reduce the risk of relapse, and enable you to manage your chronic pain effectively.
Food
As with housing, it’s important that patients have access to the nutrition they need to maintain their physical health both during and after withdrawal. This might involve pinpointing you to food banks if resources are stretched, providing nutritional guidance about a balanced diet, or teaching cooking skills.
Self help groups
Self help groups can focus around chronic pain specifically, to give you the ongoing support and advice you need moving forward. Alternatively they can focus on opioid withdrawal to support you through the process both during and after withdrawal if you feel you need it.
Self help groups tend to be small, face to face groups with other people who are going through similar struggles. Sometimes being around other people who really ‘get it’ can be invaluable. Self help can also be part of 12-step programmes for addiction, which have a set structure patients work their way through to help them sustain their withdrawal.
The WHO guidelines explain that support groups, “often provide both material assistance and emotional support, and promulgate an ideology or values through which members may attain a greater sense of personal identity.”
Activities and hobbies
Finding purpose, distraction and things you enjoy is one of the biggest motivators for both opioid withdrawal and chronic pain recovery .You may receive help to access leisure activities and hobbies, as well as support with setting goals going forward.
Building social skills
Social isolation is very common in those with chronic pain for many reasons, as well as for those with opioid dependence. When you’re not interacting socially you can lose social skills which may have come naturally previously. It can also feel anxiety-inducing to be in social situations when you have become used to being isolated. Providing social skills training can enhance confidence and equip patients with the tools they need to rebuild their social life.
Spiritual support
For those who are religious or have spiritual beliefs, providing access to this type of support is vital during withdrawal and recovery. This can enable them to feel more hopeful, strong and determined.
Cognitive behavioural therapy (CBT)
CBT works on the basis of replacing negative thought patterns and behaviours with more positive, helpful ones. CBT for opioid withdrawal focuses on changing addictive behaviours and learnt patterns of behaviour. A big part of CBT during withdrawal should be educating patients about other ways to manage their chronic pain and providing hope for the future.
For example, during CBT a patient going through withdrawal may be taught how to change dependent thinking such as ‘I need opioids or I’m never going to be able to manage my pain’, to more positive thought patterns such as ‘I can manage my pain without opioids’. They will be taught to break the association between chronic pain and the immediate need for opioids, and instead learn that chronic pain can be reduced with other natural methods.
The World Health Organization (WHO) guidelines for opioid withdrawal state that, “Cognitive approaches primarily aim to change addictive behaviours by changing faulty cognitions that serve to maintain behaviour, or by promoting positive cognitions or motivation to change behaviour.”
The aim of CBT is not only to help the patient through the withdrawal process, but to educate, prepare and equip them for the future managing their chronic pain without the use of opioids. The tools they learn through CBT can be carried forward and applied in their day to day life to reduce the chances of relapse.
Mindfulness
Mindfulness centers around being present in the moment, not allowing worries from the past or about the future to concern you. Mindfulness practices provide a deep sense of grounding, stress relief and relaxation. Mindfulness can be incredibly useful during withdrawal to help patients cope, to help them relax and provide comfort, and to enable them to sleep more deeply.
The process of mindfulness can enable patients to make more helpful choices, aiding in breaking the addiction cycle. Learning mindfulness tools can enable you to maintain a greater sense of emotional control moving forward.
Mindfulness is also very helpful in treating chronic pain, helping to break the stress and pain cycle and easing muscle tension. This equips patients with the tools to manage their chronic pain after withdrawal and to reduce the risk of relapse.
Mindfulness techniques will often be combined with medication-assisted withdrawal to bring optimal results for patients. One study found that, “those who received methadone and a mindfulness training-based intervention were 1.3 times better at controlling their cravings and had significantly greater improvements in pain, stress, and positive emotions”.
Psychotherapy and counselling
Structured counselling may be used to help patients through the experience of withdrawal and to help them gain greater coping skills for the future. Psychotherapy may also be used which is a very structured approach to dealing with problems and emotions. These talking therapies can help you to express what you’re going through and find better ways to deal with your problems.
Family therapy
Often families attend counselling together to help resolve issues which could be adding to stress. During family therapy your loved ones may learn how to support you while you withdraw from opioids and learn to help you cope with your chronic pain moving forward. This can be really useful to create a healthy, adaptive family dynamic for the patient.
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations
Coping With Withdrawal
Aside from treatments, there are other ways in which you can support yourself as you go through the withdrawal process.
Support
It’s important you have support, ideally personally as well as professionally. If you can reach out to loved ones and let them know what you are going through so that they can be there for you, this can be really helpful. The withdrawal process can be taxing emotionally as well as mentally, so having people there to cheer you on and encourage you can make all the difference.
If you find that you are struggling during withdrawal, speak to your doctor or health care team. They might be able to give you extra guidance and support to ensure you’re able to see the process through. It’s important you don’t give up, instead speak up!
Distraction
As hard as it might seem, distracting yourself as much as possible can be a great coping tool. This can help to take the focus away from pain and other withdrawal symptoms, and provide some relief. You could:
- Listen to relaxing or uplifting music
- Read a book or if you can’t focus enough to read, listen to an audio book
- Watch a fun film, TV series or a documentary
- Chat with a friend or family member on the phone
- Play video games or board games
- Do some crafts like painting, drawing or knitting
- Change environment to shift your mindset, even if it’s just walking into another room
Small, regular meals
You might not feel like eating, but it’s important that you try. Small, regular meals can be useful. Plain, bland foods are best as they are least likely to cause stomach upset. This could include toast, crackers, rice, or some fruit.
Lots of fluids
It’s so important to stay hydrated when experiencing withdrawal symptoms. Take regular small sips of water, juice or a warm drink throughout the day rather than gulping down water, to reduce the risk of vomiting. You could also choose to replace lost electrolytes with sports drinks or electrolyte replacement drinks. However, be aware these could aggravate diarrhea.
Heat and cold to manage pain
Using heat pads, wheat packs which you heat in the microwave, or a hot water bottle, can be a great way to ease muscle aches and pains. It can also be comforting and calming. Some wheat packs have a lavender scent which is comforting. Likewise, using cold packs can help to reduce inflammation and pain.
Topical analgesics
You can buy topical analgesics over the counter which are typically creams or gels which you rub onto your skin. Some create a cooling, tingling sensation and interrupt pain signals, providing some relief. Others create a heating sensation along with the same effect. Some provide a mild numbing effect to ease painful areas.
Moderate exercise
Exercising can help to provide a distraction, along with raising your mood, easing pain and muscle stiffness, and helping you to sleep more peacefully. You shouldn’t overdo exercise when you’re going through withdrawal, but some moderate exercise such as walking or stretching can be a great coping technique.
Sleep hygiene
It can be really difficult to sleep when you’re experiencing withdrawal symptoms and when dealing with chronic pain, but good sleep hygiene can help you to get the rest you need. Sleep hygiene refers to positive habits to increase your chances of sleep. This can include going to bed and getting up at roughly the same time each day; making your bedroom comfortable and relaxing; winding down before bed; and using relaxation techniques.
Remembering your end goal
There’s no denying that withdrawal is hard, so it’s absolutely vital you keep reminding yourself of why you’re doing this. You could come up with positive mantras to repeat to yourself (in your mind or out loud) to help you remember your end goal even when it’s difficult. Some examples of mantras could include: “It’s hard right now, but I can do this and it will be worth it” and “I will not give up, this is for my own good and to improve my life.”
You could also choose to focus on the future to keep you motivated: think about what you are going to do once you’ve completed your withdrawal. You could create a vision board or write down your goals to keep you focused on moving forward.
Follow Up Care
Once the acute withdrawal phase is complete, you need to learn to live without opioids. This can be tough but is possible. The post-acute withdrawal period can last up to two years: this doesn’t mean you will be experiencing severe withdrawal symptoms the whole time. It simply means you may find it difficult to adjust to life and living with chronic pain without opioids, and may experience changes in mood, anxiety, and stress levels.
The post-acute withdrawal period can lead to problems sleeping, concentrating and a decline in general mental health. It’s during this stage that you may find it most difficult not to go back to taking opioids, so it’s vital that you have the appropriate follow up care.
Maintenance treatments
Depending on your care plan and the medications used to assist you through withdrawal, you may continue to take medications as maintenance. These can include methadone and buprenorphine for example. The long term aim is to withdraw from these medications completely too.
It may appear counterintuitive to replace one opioid with another, but it’s all about a gradual withdrawal process which is manageable for the patient, with the end goal of being opioid free. Replacing an opioid which is extremely hard to withdraw from and is very addictive, with one which is less addictive and easier to withdraw from, is a step towards being opioid free.
This report from the National Institute on Drug Use explains that, “these medications do not produce a euphoric high but instead minimize withdrawal symptoms and cravings. This makes it possible for the patient to function normally, attend school or work, and participate in other forms of treatment or recovery support services to help them become free of their substance use disorder over time.”
Naltrexone is commonly used in the months after withdrawal to reduce the likelihood of relapse. As we mentioned earlier, naltrexone is an opioid blocker. It can be used after withdrawal is completed as part of an ongoing management plan to reduce opioid cravings.
Monitoring
Just as you were monitored during withdrawal, you should be monitored after your acute withdrawal phase is over. This should entail regularly seeing your doctor or someone from your health team to check how you’re doing. They should ensure you’re coping and are not at risk of relapsing. They should also signpost you to other services which may be able to help support you if you’re struggling.
Cognitive behavioural therapy (CBT)
CBT is often used as part of follow up care to help aid patients in continuing with positive coping strategies and thought processes in the long term. CBT can help patients to adjust to life without opioids, and can reduce the risk of relapse.
Introduction to other chronic pain treatment options
One of the biggest parts of follow up care is to replace the need for opioids by providing you with other chronic pain treatment options. Opioids don’t solve the problem of chronic pain, they only mask it while they’re being taken. Once you’ve withdrawn from opioids, you will be able to feel the full effects of your chronic pain again.
Patients should not withdraw from opioids and then be left in chronic pain, as understandably this exponentially increases the risk of them returning to opioids. Instead, they should be educated and signposted to scientifically proven treatments which rather than masking chronic pain, actually help them to overcome their pain in the long term.
Psychological treatments
There are a range of psychological treatments, meaning talking based therapies, which can not only help you to better manage your chronic pain, but actually reduce chronic pain symptoms. Pain neuroscience education (PNE) is a cornerstone of many of these treatments. PNE teaches you the science behind chronic pain so that you fear it less and understand why and how treatments work.
Some effective psychological treatments include:
- Cognitive Behavioural Therapy (CBT)
CBT isn’t just useful during the withdrawal process, but can actually help to treat chronic pain. Through CBT you can learn to replace negative perceptions of pain and behaviours which may be perpetuating chronic pain, with positive helpful thoughts and behaviours which actively reduce your pain levels.
- Acceptance and Commitment Therapy (ACT)
ACT helps you to let negative thoughts pass you by, teaching you that negative thoughts don’t need to lead to actions. You are then guided through committing to more positive coping strategies.
- Mindfulness
As with CBT, mindfulness isn’t only useful during the withdrawal process. It can be helpful in the ongoing treatment of chronic pain by lowering stress levels and breaking the stress and pain cycle.
- Graded Exposure Therapy
Graded exposure therapy helps patients to face their fears and movements they have been avoiding in a gradual, manageable way. The brain learns that these movements do not need to produce pain messages, therefore retraining the brain away from chronic pain.
- Graded Motor Imagery (GMI)
GMI uses imagined movements to retrain the brain gradually away from pain, teaching the brain that it no longer needs to produce chronic pain messages. These imagined movements can then be transitioned into physically performing the movements.
Manual and physical therapies
Manual and physical therapies involve movement and hands on treatment to ease chronic pain. These therapies include:
- Massage
Massage can ease muscle tension and reduce stress.
- Physical therapy
You’ll also hear this referred to as physiotherapy. This involves exercises to improve your range of movement, learning how to move your body safely, increasing your levels of functioning and strengthening your body.
- Hydrotherapy
Hydrotherapy involves doing exercises in a heated pool of water. The water takes the weight off your joints making movement easier, and the heat eases muscle pain and stiffness.
Self-management
Patients should be educated in effective self-management techniques to improve their quality of life between therapy appointments. These can include eating well; pacing activity; doing exercise; practicing good sleep hygiene; reducing stress and more.
These are just a few of the options you may be offered to replace opioids and overcome your chronic pain. You can find further details of all of your options in our pain management guide.
At Pathways, we’ve built a chronic pain therapy program that you may find useful in helping you to manage, and reduce your pain. You can find download links below.
Opioid use in the future
While once you withdraw from opioids it’s important not to restart them for chronic pain, in the future there is a chance that you may be offered opioids for acute pain if you have an accident or injury. In this circumstance it’s always a good idea to speak up and explain your past situation to medical staff.
If you were able to successfully taper off your opioids and have maintained this, your doctor may monitor you more closely but it may be safe for you to take opioids in the short term. If you struggled with addiction and found withdrawal very difficult, or have had relapses, your doctor may look at alternative pain control.
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations
References
Christine Case-Lo, (2019), “Withdrawing from Opiates and Opioids”. Healthline.
National Institute on Drug Abuse, (2020), “Prescription Opioids DrugFacts”.
Marion Lee, MD, Sanford Silverman, MD, Hans Hansen, MD, et al, (2011), “A Comprehensive Review of Opioid-Induced Hyperalgesia.” Pain Physician 2011; 14:145-161.
Mayo Clinic, (2020), “Tapering off opioids: When and how”.
World Health Organization, Department of Mental Health and Substance Abuse, (2009), “Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence”.
National Institute on Drug Abuse, (2020), “Medications to Treat Opioid Use Disorder Research Report”.
Sarah Wakeman, MD, (2018), “Lofexidine: Another option for withdrawal from opioids, but is it better?” Harvard Medical School.
National Institute for Health & Clinical Excellence, (2008), “Drug misuse: Opioid detoxification”.
Rutgers University. (2019), “Mindfulness may reduce opioid cravings, study finds: Opioid users, chronic pain sufferers may experience fewer relapses and greater well-being.” ScienceDaily.