Graded Motor Imagery (GMI) is used for complex pain and movement problems. It’s a process of training your brain away from pain using specific imagery (imagined or real). For example, did you know that simply imagining moving a painful part of your body, pain-free, helps to train your brain to stop creating pain?
GMI is backed by the latest pain science. For example, this study found that,
Pain intensity decreased over the course of GMI, and relief was maintained at follow-up
What is graded motor imagery?
Our brains are neuroplastic, which simply means that they constantly change and adapt from the experiences in our lives. This study states that, “Local cortical connections and responses are continuously reorganized as a result of peripheral and central alterations of input.” In other words, everything you do, and everything you don’t do, shapes your brain.
When pain becomes chronic, it literally changes the way that the brain and the nervous system work. Your brain and nervous system learn pain, and the more you experience pain – the greater the chance of pain striking again as your pain system is stuck in a state of high-alert – this is also known as central sensitization.
Just as this neuroplasticity has worked against pain patients to create this ongoing cycle, so it can be used for them, to break the cycle and get past pain! GMI targets different areas of the brain which process and create this pain and essentially ‘re-teaches’ these areas of the brain to react in an adaptive way.
The word ‘graded’ simply means that it is done in a step by step way. With pain patients it’s important to work at a pace that allows them to challenge their pain without causing a flare up in symptoms; with GMI patient’s can move at a pace that works for them individually.
The word ‘motor’ refers to movement of the body. ‘Imagery’ refers to using visualisation, as GMI uses images to guide patients through imagined movement and to tackle situations that might usually evoke pain. This study explains that,
Imagery refers to the “creation (or re-creation) of any experience in the mind—auditory, visual, tactile, olfactory, gustatory, kinesthetic, organic.
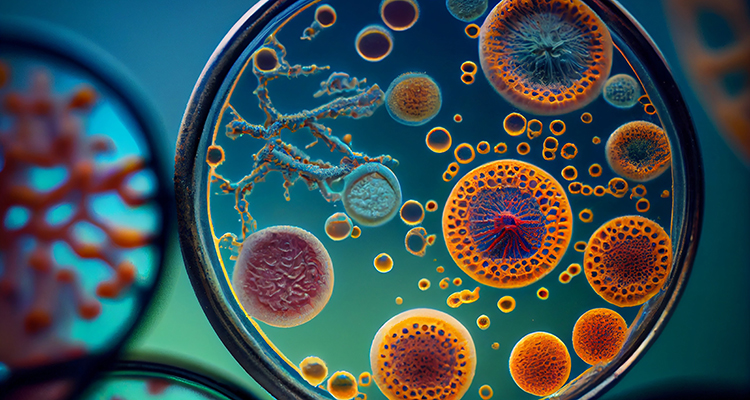
All pain comes from our brain
The first thing to understand is that all pain comes from our brains; we have neurotags in our brain which are networks of interconnected neurons or brain cells within the brain. When neurotags are activated, they produce a sensation or experience. In the case of pain, these neurotags send signals through our nervous system instructing the body as to when pain needs to be felt and in which areas of the body.

When pain becomes chronic, the neurotags which are specifically producing the chronic pain become sensitized to pain, meaning they are habituated to creating that pain and will continue to do so without inhibiting it. Basically creating that pain becomes that neurotags job and so they become overactive, resulting in you experiencing persistent pain.
This applies to any type of pain whether it’s acute for example from an injury, or chronic. Saying that pain comes from the brain does not imply that your pain is not real or not valid. Understanding this concept is the first step to understanding how pain can be treated with GMI or other methods.
Why is GMI graded?
Graded motor imagery is graded in two ways; firstly it is broken up into three stages, all of them different, impliticately researched and shared in a very specific format to produce the best results for patients. Research has suggested that the order of these sessions is important for the successful outcome and reduction of pain. This study explains that, “these stages are designed to optimize sensory-motor processing and gradually engage the cortical motor networks without triggering the protective pain response.”
Secondly GMI is graded in order to ensure that it’s manageable for the patient; the goal is to build up imagined movement and actual movement slowly so that a flare up in the patient’s symptoms does not occur. A flare up would work against the treatment; it’s important that the patient is working at a pace that works for them individually to produce the best results.
What are the three stages?
Left/right discrimination
Research shows that people who are in chronic pain can lose the ability to distinguish between their left and right side when looking at images of the parts of their body where pain is experienced. The mental map we have of the body can start to become distorted.
When chronic pain patients look at pictures of parts of their body, they react much more slowly and less accurately when trying to pick out which body parts belong to the left and right side respectively.
Before patients can move on to successfully visualizing parts of their body moving in specific ways, they need to be able to discriminate between the left and right sides of the body. This stage of therapy builds patients ability to correctly identify left and right sides of the body.
Usually flash cards or pictures are used during this stage to represent body parts; computer programmes, apps, or even magazine pictures can be used. This works by challenging patients during the therapy to quickly identify the left and right body parts or body movements. For example, do you identify the following foot as a left foot or right foot?

This stage of the therapy will usually be done for a set amount of time each day, until the patients are able to quickly identify left and right sides of the body. As for the image above, it’s the left foot 🙂
Explicit motor imagery
A quarter of the neurons in the brain are referred to as ‘mirror neurons’, which means that they start sending signals out even when you are just thinking about moving or when you watch someone else move.
When you imagine your body moving in a specific way, the same neurotags are activated for that specific movement as when you are actually performing the movement. This means that even imagined movements can cause pain, but it also means that we can use this to our benefit during this stage of GMI. This study explains that, “Motor imagery is the mental execution of a movement without any overt movement or without any peripheral (muscle) activation.”
GMI takes you through imagining your body engaging in certain movements which usually evoke pain without actually performing the movement. This typically starts off with the patient learning how to practice a deep visualization relevant to the affected part of the body.
The patient will then proceed to imagine the limb moving in a specific way. Often the required movement will be indicated by a picture or animation to prompt the patient and help them imagine the movement appropriately. Sometimes flash cards, magazines, computer programmes or apps can be used, as with the left/right discrimmation stage.
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations
This is done in a graded way, starting from a movement that causes minimal pain. If the pain neurotags are activated during the imagined movement, then the therapy will focus on a smaller movement with less pain or make the session shorter, so that it is in bite sized pieces and is more manageable.This method isn’t linear, meaning if there is an action that causes pain, then the patient can redo earlier stages to address it.
For example, if walking across the room usually evokes pain, GMI helps you to imagine getting up from your chair, then once the brain has been taught that this action shouldn’t be causing pain, the imagery can move onto imagining moving your legs, walking forward, and progressively continue until you have imagined reaching the other side of the room.
Once your brain has learnt that this action shouldn’t be associated with pain, like many patients, you may be able to walk across the room pain-free! Your brain and nervous system learn that the protective pain response is no longer required.
This study explains that,
Graded motor imagery (GMI) utilizing various tactile and cognitive processes has shown efficacy in decreasing pain, disability and movement restrictions in musculoskeletal pain.
Mirror therapy
When you put a mirror in front of one half of your body and hide the other half behind it, you can trick your brain into reducing pain sensitivity. For example, if you place your pain-free right hand in front of a mirror box, and hide your left hand within the mirror box, you can trick your brain into believing that the reflection is indeed your left hand.
Now, when you move your pain-free right hand, it looks like your left hand is also moving but pain-free. This can be a powerful way to reduce pain.

Mirror therapy activates the brain less than actual movement but more than imagery, which is why it is the final stage. Any mirror can be used for this but there are specific mirror boxes which can be used for this specific purpose.
Once these three stages have been successfully completed, the patient is able to move onto actually performing the movements that they have retrained their brains to engage in without pain.
How can GMI help with chronic pain?
GMI can help you with your chronic pain in many ways by:
- Helping you to gain a deeper understanding of how your pain works.
- Helping you to understand that your pain is not going to ‘damage you’
- Increasing confidence through understanding and education.
- Empowering patients to take control of their life once again and to actively be involved in treating their own pain symptoms
- Allowing you to experience relief from your pain when you are both resting and exercising, increasing your level of functioning and allowing you to rest properly! This study states that, “GMI is an effective treatment in decreasing pain levels both during rest and activity.”
- Helping you to maintain this reduction or elimination of symptoms for the long term; this study which tested GMI found that, “The results pointed to a significant and substantial reduction in pain related to the intervention and an increase in function of the involved limb, which was maintained at a 6-month follow-up.”
- Aiding patients in overcoming fear and avoidance behaviours.
- Being cost effective treatment
- Not creating side effects or many adverse effects as explained here.
- Being non-invasive, meaning that it does not involve surgery and is not harmful.
- Being flexible, able to be used alongside physical therapy, mindfulness therapies, medications and other treatments.
How can you access graded motor imagery?
A lot of doctors may not yet be aware of this sort of treatment so it can be tricky to access it through medical professionals. However, online resources (such as this post and our app) (update Aug 2023: Pathways is now a web app! Start our program here) can help you get started and practicing in your own time.
Graded motor imagery can help you to get your life back, it can allow you to get your symptoms under control and even live a chronic pain free life! It takes courage and consistent work, but it’s so worth it!
References
- The Clinical Journal of Pain, Volume 29, Issue 3, p 276–279, Walz, Andrea D. MSc., Usichenko, Taras MD, Moseley, G. Lorimer PhD., Lotze, Martin MD, (2013), “Graded Motor Imagery and the Impact on Pain Processing in a Case of CRPS”
- Physiotherapy Theory and Practice, Volume 31, Issue 7, Adriaan Louw, PT, PhD, Stephen G. Schmidt PT, MSc, Colleen Louw,PT, MPT., Emilio J. Puentedura , PT, DPT, PhD.,, (2015) “Moving without moving: immediate management following lumbar spine surgery using a graded motor imagery approach: a case report”
- Physical Therapy, Volume 87, Issue 7, Ruth Dickstein, Judith E Deutsch, (2007), “Motor Imagery in Physical Therapist Practice”
- Lorimer Moseley, David S. Butler, Timothy B. Beames, Thomas J. Giles, (2012), “The Graded Motor Imagery Handbook”
- Journal of Neural Transmission, Th. Mulder, (2007), “Motor imagery and action observation: cognitive tools for rehabilitation”
- Journal of Hand Therapy, Volume 31, Issue 1, Burcu Dilek, PhD, PT, Cigdem Ayhan, PhD, PTb, Gozde Yagci, PhD, PTb, Yavuz Yakut, PhD, PT, (2018), “Effectiveness of the graded motor imagery to improve hand function in patients with distal radius fracture: A randomized controlled trial”
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations