Stress and chronic pain are far more intertwined than you might think; one can cause the other and you can become stuck in this cycle which is increasingly hard to get out of, but it is possible to break free!
What is stress?
Stress itself is a normal part of life; you become stressed when you face hard situations in your lives or when you have a lot to deal with. There are many reasons someone may experience stress; it’s the way our brains make us aware that there’s something we may need to deal with and subsequently gets us ready to take action.
Essentially stress is there as an early warning system, just like pain; it functions to alert you to what is happening in your environment and to help you get a handle on things, in a similar way as acute pain lets you know that something is wrong. This study states that, “Pain and stress are both adaptive in protecting the organism” and goes onto explain that when these processes become chronic, meaning that they become ongoing and persistent, then they become maladaptive, meaning that they are not adjusting to the environment appropriately.
Stress puts the body into a ‘fight or flight’ mode, getting you ready to tackle any danger or adverse situation which may be present. When they function as they should, stress and pain are a positive addition to your life, helping to keep you safe.
However, when stress is prolonged, it becomes harmful and negative, as does pain. Pain and stress are only designed to alert the body on a short-term basis, and the body is only designed to deal with them for a short amount of time. When the body is stuck in that ‘fight or flight’ mode for an extended period, this overworks the body and causes problems.

Having that support there has also been shown to reduce the fear of their condition; often people will avoid certain situations because they are worried about how their actions may affect their symptoms, which in fact compounds their symptoms. With support by their side people are more likely to engage in activities and to feel less afraid. This study indicates that, “the presence of a supportive other may diminish one’s appraisal of threat, which in turn might influence one’s experience of pain by reducing the negative emotions and expectations of pain”. The same study also suggests that loved ones may distract the patient’s brain away from their pain more so, and without that focus on the pain solely and with something more positive to focus on, symptoms can diminish.
Being in a happy romantic relationship with a supportive partner has been proven to have really positive impacts on health, even for those without any health conditions, such as improving mental health as well as physical health as shown in this book.
The connections we have in our lives are far more impactful on our health than we may be aware; your position in supporting a loved one with a chronic condition is significant, and you are important in that process. You are not helpless, even just maintaining that good connection with them is so much more helpful than you might be aware of.
What does stress do to the body?
When you become stressed the body moves into a state of high alert, so that you are ready to take action where it might be needed. The hypothalamic-pituitary-adrenal axis (HPA), is the area of your brain that interacts with your environment and when stress is detected, it starts to release the hormones that tell other areas of your brain to prepare the body for action. These hormones essentially start to get the body ready for ‘fight or flight’. When stress is present, the autonomic nervous system which is the part of the nervous system which controls things like blood pressure and blood flow, joins in and jumps into action to help prepare the body.
Basically, this means that your blood pressure and heart rate rise. Blood flows to the areas of your body that are going to be needed to either fight or flight, and therefore less blood flows to organs that are deemed to be less of a priority, such as blood flowing away from your digestive system. Your immune system will be lowered because it isn’t a priority where there is immediate danger. Muscles tighten ready for action; your breathing may get faster; adrenalin levels increase as do your blood sugar and cholesterol levels.
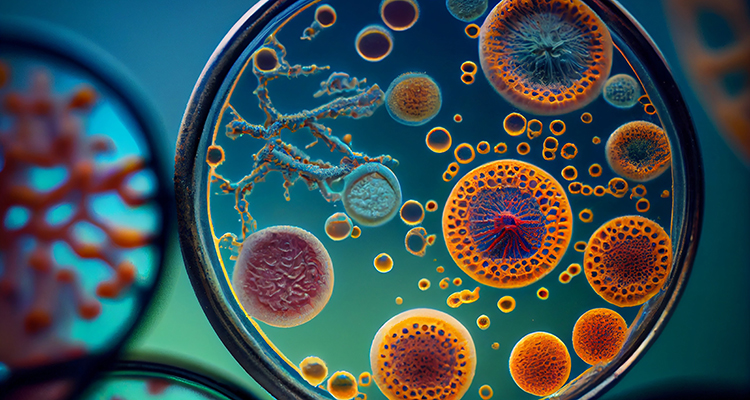
Cortisol is one of the main hormones which is released, sometimes even called the stress hormone. Cortisol is usually released during the day in a steady fashion when there is no stress present, working to maintain the correct blood flow to the vital organs in the body, to control the glucose in your blood and to essentially make sure that your body is functioning in the way it’s supposed to. It also controls inflammation, as this article explains,
Cortisol is also a potent anti-inflammatory hormone; it prevents the widespread tissue and nerve damage associated with inflammation.
When stress comes into the picture cortisol is then released more so, doing its job to get the body ready to deal with the stressor; this is an adaptive reaction, meaning that it is an appropriate reaction to what is happening in the environment. However, when cortisol is released for prolonged periods, it becomes maladaptive, meaning it is not an appropriate reaction and detrimental to the body. It is then actually doing the opposite of what it is supposed to, becoming a cause of inflammation and exacerbating the stress and fear response. This article emphasises the damage this can do to the body, stating that,
excessive or prolonged cortisol secretion may have crippling effects, both physically and psychologically.

If this situation is ongoing then it can really take its toll on your body. Understanding how the ongoing stress response affects various areas of the body can help you understand your symptoms, and take action:
- Heart
When your heart rate is increased, it in turn raises your blood pressure. Blood pressure is the rate at which the heart is working to push blood around your body and when your heart is overworking, it is under strain that it is not designed to withstand in the long term. You may feel your heart racing and even feel shaky and confused as a result. This can lead to damage to your system and problems with your heart.

- Lungs
When you are breathing quicker over a long period of time, this hyperventilation is sending extra oxygen into your bloodstream which then isn’t being used because you aren’t acting on that fight or flight response. This excess of oxygen in the blood can cause you to feel dizzy and jittery. It can also cause you to feel pain in your diaphragm because your lungs are working too fast. Breathing too fast can irritate your airways and cause issues for those with asthma and similar breathing problems.
- Eyes
When adrenaline, one of the hormones which readies your body for this stress response, is sent into the bloodstream, your eyes dilate so that your vision can be improved. When this is long term this can overwork your eyes, causing blurry vision, ticks in your eye and general muscle tiredness around the eyes.
- Mouth
When you’re in this state of stress you might find that your mouth is very dry, as your body sends resources elsewhere; as a result, you may find it difficult to swallow. The tension you feel may be presented as you grinding your teeth or clenching your jaw, in turn putting even more pressure on the muscles in your mouth. I tend to find that I grind my teeth a lot without being aware, which is something I find hard to combat.
- Ears
During stress your ears are on high alert, so when the stress response becomes chronic, then this can make you very sensitive to sound. This is something that I experience with fibromyalgia; it can be very uncomfortable and overwhelming when noises feel too loud.

- Immune system
- Digestive system
- Skin
- Bones
- Muscles
- Emotional state
Your body is sending resources elsewhere during a stress response and so your immune system is lowered; over a longer period this means that you are more likely to get diseases and viruses as your immune system is not protecting you as it should.
Without the resources it needs, the digestive system struggles to function. You may experience this through bowel problems such as constipation or diarrhoea; IBS is common with fibromyalgia and other chronic conditions. Your digestion is slowed and issues such as heartburn and indigestion are common.
Stress causes your skin to be more sensitive and reactive, often leading to skin problems such as rashes, itching, acne and being more prone to spot breakouts.
The excess cortisol that is sent into your bloodstream can cause problems with the building blocks in your body; the cells that build new bone tissue are not getting the resources they need, so as a result, your bone density is reduced.
In order to be ready for action your muscles will be tightened and overworked during chronic stress. This can cause pain and even slower reaction times.
All this tension and change within your body tends to have a big impact on emotions and mood. It can make it hard to sleep, hard to concentrate, cause problems with sex drive, and can lead to mental illness like anxiety and depression.

How do stress and chronic pain influence each other?
The body being in this high state of stress can cause pain in and of itself, as well as exacerbating pain. The muscles tightening and the body being in a constant state of stress takes its toll on the body physically because it is not designed to cope with being in this tense state for a long period of time. The overproduction of cortisol we discussed can cause inflammation in the body, as well as causing pain and fatigue. This article concluded that,
sustained endocrine stress response observed in individuals with a smaller hippocampi induces changes in the function of the hippocampal complex that may contribute to the persistent pain states.
Once you are experiencing pain, it’s common for patients to start worrying about that pain. Normally pain is a warning response, so it’s natural to be concerned. Often patients will worry about what could be causing the pain and focus on ways that they can avoid situations that either initially caused the pain, that have in the past made their symptoms flare, or even that they feel could potentially increase their pain. For example, if you have gone out walking and that has made your symptoms flare, you may then avoid exercise because you feel it is going to result in you being in more pain.

You can end up avoiding situations that you feel are going to make your pain worse, such as refraining from exercise and moving your body; this can feel as though you are protecting yourself and it seems like a logical response when in fact, it contributes to keeping you in this pain and stress cycle. By not moving your body, your muscles are not getting the use they need, and therefore become weaker.
The fear of being in pain, the avoidance and anticipation of pain, causes stress in itself and then we’re back to stress causing pain. This is known as catastrophizing about your pain, simply meaning that you are focusing on it and worrying about it excessively, sometimes even before it has happened, and therefore you change your behaviour in accordance. This change in behaviour is proven to increase your pain and keep you stuck in this cycle. This study found that, “Catastrophizers reported more negative pain-related thoughts, more emotional distress, and more pain than noncatastrophizers.”
Chronic pain and chronic stress change how your brain and nervous system work, which is known as central sensitization, wherein your nervous system is in a constant state of overdrive. This is an ongoing cycle where pain causes stress and stress causes pain, and so it continues.
How to break the cycle
It’s important that you know that these reactions are completely natural; to try and protect yourself in what feels like the most logical way is understandable. It’s important to know that the pain you are going through is not your fault, and it is entirely valid. Understanding the cause of your pain and focusing on the science behind this cycle gives you the upper hand in the battle against your pain, allowing you to understand where you can redirect that focus and positively change things with new coping strategies.
So, let’s go ahead and look at the more positive side of things; how you can break that pain and stress cycle and improve your life! Breaking the cycle is about replacing maladaptive behaviours with adaptive behaviours. Remember that you don’t have to do this on your own; there are lots of therapies and help out there which can aid you; you can find more information about how to get help later in the article.
- Educate yourself about the pain cycle
Understanding what is causing your pain, the science behind how your pain works and why you need to change your behaviours is a great foundation to start from. This understanding can help you to realise that you are not in danger and that your pain is not going to harm you, which gives you more confidence going forward with breaking the cycle.
Knowledge about your condition allows you to realise why you need to change things and the benefits of doing so, giving you that motivation and clarity you need to push forward. There’s a lot of information to be found online, in books, in leaflets and from professionals.
- Replace avoidance with action!
Avoiding situations because you are worried about the effect it will have on your chronic pain is actually making your pain worse rather than better. Once you understand the science behind it, you can see why it’s so important to change this. Instead of avoiding situations, you can start to face that fear head on.
You don’t have to do this all at once and no one is suggesting it will be easy but facing situations you have been avoiding in a gradual way at your own pace, is going to really help you to break that cycle.
- Exercise
One of the main things chronic pain patients tend to avoid or feel that they cannot do is exercise; starting to find ways to gently exercise on a regular basis is really going to break that cycle! Again, you can do this at your own pace. Gentle exercises like walking, swimming and even physical therapy with help from medical professionals, can help you to get your body moving. It may feel worrying at first and may sound counterproductive, but it truly does help to break the pain cycle.
From personal experience, starting with gentle walking at stage when I could barely walk across the room and would use a mobility scooter often because I thought I couldn’t exercise with my pain, to being able to do a sponsored hike of nine miles, I can attest to the benefits of exercise on getting out of the pain cycle.

- Eating a healthy diet
Ensuring you are giving your body the fuel it needs to function in the best way possible is setting yourself up for victory against your symptoms. Avoiding things like alcohol, smoking and fatty foods can really help. Again this doesn’t have to be something you have to do all at once, and nobody is perfect, but trying to make your diet as healthy as possibel will help you beat pain. Even small changes such as reducing one bad habit, or replacing one food with a healthier alternative is a great place to start.
- Socialize
Maintaining social interactions is a great way to combat this cycle; it’s often something that people with chronic pain conditions tend to avoid. Ensuring that you are proactive in being social can be very helpful; it can also be a lot of fun! Friendships and relationships are important and it’s easy to forget that when you’re struggling; let people be there for you and allow yourself to enjoy social experiences.
- Distract yourself
Focusing on pain can amplify it and increase stress around it; it’s hard to distract yourself from pain especially when it’s severe, but it does get easier the more that you practice distraction. Actively distracting yourself with other things, whether that be the exercise we have mentioned or doing something you enjoy, anything that keeps your mind from dwelling on the pain is really effective in turning down the volume on pain.
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations
- Maintaining a routine
- Having a good sleep routine
Feeling that you are not able to function is common and often people with chronic pain are out of work. No one is suggesting that your experience is not valid and that you should click your fingers and go back to work, but learning how to tackle your pain in a step by step way and aim for those sort of goals is going to help you break free from this cycle.
Maintaining a routine, whether that means working or doing other things that keep your busy throughout the day, helps you to keep your body moving, to keep your mind focused on productive things and aids in keeping your mood stable.
Ensuring you are doing all you can to sleep well is going to aid your body and mind in functioning well. This is often easier said than done with chronic pain but the more you try to maintain that routine the better. Things like winding down for bed and relaxing before bedtime are valuable. Going to bed at the same time every night and getting up at the same time in the morning even if you haven’t slept well, can help your body clock to get in sync. Keeping busy during the day and doing exercise to help your body feel tired enough for sleep is beneficial.

- Dealing with stressors
Focusing on reducing stress in life, dealing with the root causes of the stress, is in turn going to reduce your pain and the effect this cycle has on your life. You can’t always control the things that are causing you stress but learning to deal with them more proactively such as using mindfulness, using talking therapies, talking to those around you, asking for support and using healthy coping mechanisms, can be helpful. Where there are things that you can change, focusing on a step by step plan to actively deal with the cause of your stress is a great way to be proactive.
Where can I get help to break this cycle?
You don’t have to try and break this cycle alone; the thought of all of this can be very overwhelming but don’t panic! There are plenty of ways that you can get help to start breaking the cycle.
- Advocate for yourself with medical professionals
Seeking a diagnosis and asking for the help you need is really important; unfortunately you may face stigma with medical professionals in relation to chronic pain, but do not let this stop you. Advocating for yourself and pushing for the diagnosis and treatment that you need is important. You can call hotlines for more advice or take a loved one with you, so that you have support in standing strong and advocating for yourself.
- Ask friends and family for help
Asking those around you to help you to exercise, to eat in a more healthy way or to socialize more can be really helpful. Often doing things with someone you trust rather than on your own can really give you that motivation to keep going, making it less daunting and can even make it fun!
- Physical Therapy
You may be able to see a physical therapist through your doctor or of your own accord, someone who can help you to learn how to move your body in a way that works for you. They can work with you to build up your strength and learn how to work around your limits.
- Mindfulness
Learning how to practice mindfulness and utilize tools like meditation can help you to relax and feel in a much more peaceful place emotionally, enabling you to be better equipped to deal with your pain.

- Acceptance and Commitment Therapy (ACT)
ACT can help you to really accept what is happening within your body regarding your pain and understand that you can still function even with your pain; it does not have to limit you. You can receive ACT from a medical professional or through an online source.
- Cognitive Behavioural Therapy (CBT)
Engaging with CBT can help you to understand your pain and actively replace negative thoughts and behaviours with positive ones; it can really guide you to breaking this cycle and taking that power back. You can seek CBT from a doctor, from a private therapist in a face to face setting or online through an app like ours (download links below) (update Aug 2023: Pathways is now a web app! Start our program here).
Fundamentally, even though it can be hard to break that stress and pain cycle, it can be done. It isn’t a linear process, it doesn’t have to happen all at once; you can take it one step at a time and get the help that you need in order to take your life back. Your pain does not have to control your life; you are the author of your own story, and you can start to believe that again.
Please note: This article is made available for educational purposes only, not to provide personal medical advice.
References
- Chadi G Abdallah, Paul Geha, (2017), “Chronic Pain and Chronic Stress: Two Sides of the Same Coin?”
- Brain, 136(Pt 3):815-27,Vachon-Presseau E, Roy M, Martel MO, Caron E, Marin MF, Chen J, Albouy G, Plante I, Sullivan MJ, Lupien SJ, Rainville P, (2013), “The stress model of chronic pain: evidence from basal cortisol and hippocampal structure and function in humans.”
- Life Counselling Centre, Cindy R Nelson RN-BC, MA, BSN, CAAPM, “Understanding the Pain-Stress Cycle”
-
Physical Therapy, Volume 94, Issue 12, Pages 1816–1825, Kara E. Hannibal, Mark D. Bishop, (2014), “Chronic Stress, Cortisol Dysfunction, and Pain: A Psychoneuroendocrine Rationale for Stress Management in Pain Rehabilitation ”
- Brain, Volume 136, Issue 3, Pages 815–827, Etienne Vachon-Presseau, Mathieu Roy, Marc-Olivier Martel, Etienne Caron, Marie-France Marin, Jeni Chen, Geneviève Albouy, Isabelle Plante, Michael J. Sullivan, Sonia J. Lupien, Pierre Rainville, (2013), “The stress model of chronic pain: evidence from basal cortisol and hippocampal structure and function in humans”
- Sullivan, M. J. L., Bishop, S. R., & Pivik, J. (1995). “The Pain Catastrophizing Scale: Development and validation”
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations