Living with chronic pain is by nature worrying, but when this worry becomes excessive, it can make your physical experience of pain a lot worse
What is pain catastrophizing?
A little bit of concern about your pain is natural and doesn’t present a problem. But if you find yourself constantly worrying about the pain, and thinking the worst, you’re ‘catastrophizing’. Every time you do this it signals more danger to the brain (which creates all pain) and as a result, you’ll feel more pain more often.
This study defines pain catastrophizing as, “a persistent pattern of distressing cognitive and emotional responses to current or anticipated pain.“
There are two important things to understand, the first is that this isn’t your fault; worrying in response to pain is a logical response. The second is that you can learn to change it.
Three pain catastrophizing components
There are three parts to catastrophizing about your pain: not everyone will experience them all and they will vary in severity. You may experience different aspects on different days, depending on what is happening in your life and how you are experiencing your symptoms, as explained here, “It is likely that the experience of catastrophic thoughts varies as a result of day to day fluctuations in symptom severity and other pain-related contextual features.”
- Rumination: this simply means that you cannot get the pain off your mind. You may be constantly thinking about how much it hurts, feel unable to distract yourself or focus on anything else.
- Magnification: this means you may be focused on events that haven’t even happened yet, thinking about how much worse they could potentially make your pain, or be worrying about how your chronic pain condition is going to worsen over time. For example, you may think, “this pain is only going to get worse, then I won’t be able to work, then I won’t be able to support my family” and so on, even if these beliefs are not based on facts.
- Helplessness: this involves feeling as though you are not in control of your pain, that it is running your life. You may feel that there is nothing you can do to improve your life or your symptoms, essentially that there is no hope.
How does catastrophizing affect chronic pain?

Pain catastrophizing has been proven to worsen pain, to increase disability, decrease functioning, and worsen mental health, as explained here. The study also found that, “pain catastrophizing accounted for up to 31% of the variance in pain severity” Let’s look at how and why catastrophizing affects chronic pain in such a severe way.
- Increased stress
Being in a constant state of worry can result in stress levels rising. As all know, that’s detrimental to the body which is not designed to cope with the effects of stress for prolonged periods. Stress makes the body fatigued as it’s over worked, constantly stuck in a state of ‘fight or flight’. Stress keeps muscles tense, suppresses your immune system, and increases inflammation as well as pain; this becomes a cycle of stress causing pain and pain causing stress.
- Fear avoidance
Anticipating pain getting worse with activity can lead to fear of movement, also called kinesiophobia; you may begin to avoid situations which you feel could worsen your pain as a result of this fear. As you avoid activity, your body becomes deconditioned meaning your muscles weaken. This makes further activity harder as your body is not prepared for it, which reinforces to your brain that your worries were ‘right’ because the activity did cause pain. This study explains that, “catastrophic misinterpretations in response to pain (i.e., imagining the worst possible outcomes) lead to fear of activity and subsequent avoidance.”)
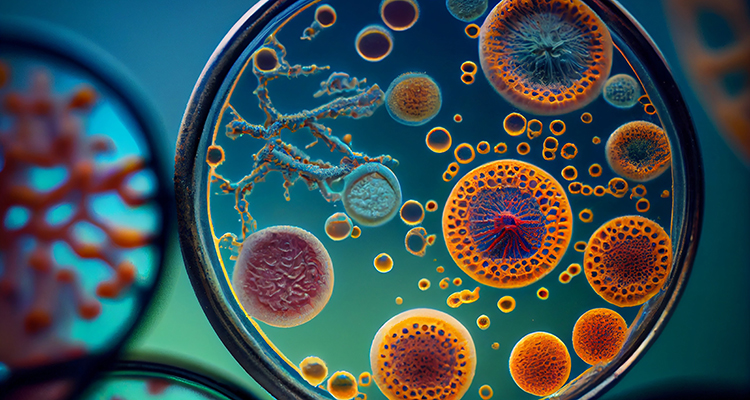
- The brain learns pain
Our brains are neuroplastic which means they learn from what is happening in our environment and what our bodies experience. Chronic pain changes our nerve pathways, meaning that our brain learns that it ‘should’ produce pain in certain situations, when in fact it isn’t needed. Our nervous system becomes overactive, also known as central sensitization.
This study explains this well: “pain catastrophizing might be associated with diminished endogenous inhibition of pain coupled with central sensitization, which may represent a CNS (central nervous system) mechanism by which pain catastrophizing is associated with the development, maintenance and aggravation of persistent pain.”
This study states that the same areas of the brain which process the catastrophizing, also produce and control pain signals, meaning that they can activate and influence each other: “pain catastrophizing, in both healthy volunteers and pain patients, is related to greater activity in areas implicated in affective processing of pain”
By anticipating and worrying that certain actions are going to worsen your pain, you are reinforcing to your brain that these situations ‘should’ cause pain. So the way your nervous system and brain is working is changed, as explained here; the brain has learnt that it should create pain messages for the activities you are worried about and doesn’t inhibit pain.
This study looked at the ways that our nervous systems can control the pain we experience, and found that, “individuals with high catastrophizing levels demonstrated higher pain intensities and lower effects of DNIC (the process we use to modulate and control pain) indicating that catastrophizing might have a significant impact on pain perception via an association with pain modulation.”
- Exaggerated muscular responses
Catastrophizing about a specific area of the body being in pain can affect the responses of the muscles in that area. For example if you have chronic pain in your neck and are intensely focused on this area of your body, it can cause the muscles in your neck to be overactive, tense and more painful, as explained here, “pain catastrophizing might be related to greater chronic low back pain severity and disability via specifically exaggerated muscular responses near the site of injury”
- Less or more likely to seek help
Those who catastrophize about their pain tend to be at one of two extremes when it comes to seeking help for their pain. Due to the fear of movement and the fear of what doctors may ‘find’ during appointments, those who catastrophize about pain may be less likely to seek help. However some people who catastrophize frequently visit their doctor in excess, as explained here.
- Mental health
Feeling constantly worried about your pain and being unable to engage in regular day to day activities can take a real toll on your mental health. Anxiety can develop or be worsened; often the feelings of helplessness, being unable to focus on things that you enjoy and the pain being all consuming can lead to depression.

Who is affected by pain catastrophizing?
Anyone can be affected but some research does suggest that certain factors make you more likely to struggle with pain catastrophizing. Women seem more likely to catastrophize about their pain than men, possibly to do with the way their nervous system works, as explained here.
Pain patients of any age can be prone to catastrophizing, but it seems that there are some differences between younger and older patients in regards to why they worry, as explained here, “in younger adults, catastrophizing is associated with emotional response to pain while in older subjects, it is preferentially associated with the actual pain intensity.”
There is research that suggests that genetics play a part in whether you are more predisposed to catastrophizing; research has found that certain genes that cause more worry and fear, as well as some which affect the way an individual perceives pain. More research needs to be done into the exact genes which can be linked to catastrophizing as explained in this study.
Our personality can affect how we deal with and perceive pain; we’re all individual and some of us are more inclined to worry in general. Our environment and lifestyle can affect whether we are more likely to catastrophize; those who have mental health difficulties previous to or comorbid with their chronic pain, and those who experience more stress in their lives, are more likely to catastrophize.
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations
Our personal understanding of the science behind pain also has a big influence on how we perceive pain, as this study explains. The study also goes on to explain that the experiences we have around pain during our formative years can influence whether or not we are likely to catastrophize. For example, if you have experienced a very painful situation in your early life, you are likely to have the association that all pain is going to be severe and very scary. On the other hand, if you have grown up around someone with chronic pain who doesn’t catastrophize, you are more likely to develop healthy coping strategies and harbour less worry about pain.
The social connections we have in our lives affect us more than we may realise; those of us with healthy and secure connections in our lives are less likely to catastrophize. Previous experience of insecure attachments, trust issues and lack of confidence socially can contribute to the likelihood of catastrophizing. This study states that, “rejection anxiety and beliefs of personal unworthiness associated with fear avoidance while discomfort with intimacy and interpersonal mistrust is linked strongly with pain catastrophizing.”

The Pain Catastrophizing Scale
In order to establish how severe your level of pain catastrophizing is and how much it’s affecting your pain levels and daily functioning, a scale is typically used based around the three concepts we mentioned earlier: rumination, magnification and helplessness. Patients are asked to score 13 negative thoughts about pain on a sliding scale of 0 (not at all) to 5 (all the time) for example, indicating how often you experience those thoughts and how they affect you.
The doctor will also discuss other symptoms, your lifestyle and clinical history; from there, the appropriate treatment can be recommended.
What treatments are available?
Pain catastrophizing can be tackled and overcome, allowing you to gain real reductions in persistent pain. There are many types of therapy that can help, it’s about finding what you feel will work for you. You can access these therapies through your doctor or specialist; if you are unable to get access to them through your doctor or need access to treatment sooner than it’s offered, you could seek them through a private practitioner or online through a pain therapy app likes ours (update Aug 2023: Pathways is now a web app! Start our program here).
- Talking therapies
Counselling to deal with anxiety and depression can help to reduce the feelings of helplessness that come with pain catastrophizing, and put you in a better mental state to begin other therapies directed towards your catastrophizing as explained here.
- Cognitive Behaviour Therapy (CBT)
CBT helps you to change how you think about your pain. A CBT therapist can help you to look at the evidence behind the negative thoughts you are having, helping you to see that they are not based in fact. CBT helps you to replace those negative catastrophizing thoughts and behaviours with positive thoughts and behaviours; this study explains that, “a core component of multidisciplinary pain treatment is often cognitive–behavioral techniques involving reducing catastrophizing and enhancing adaptive pain-coping skills.”
CBT can give you the tools to relax your mind and to focus on other things instead of your pain; it can help you to feel empowered and in control instead of feeling that your pain is controlling you!
- Acceptance and Commitment Therapy (ACT)
Instead of focusing on changing the way you think about pain, ACT helps you to realise that a negative thought about your pain is just a thought; that thought doesn’t have to progress into catastrophizing but at the same time doesn’t need to be pushed aside. It allows you to think something negative, and then move on, taking the power away from the thought and not allowing it to influence your behaviour.
- Mindfulness
Techniques like meditation, guided imagery and visualization can reduce stress and promote relaxation; stress and pain influence each other so by reducing stress in your life, your symptoms can be reduced in accordance.

- Graded motor imagery (GMI)
GMI works to retrain the brain away from pain, using imagined movements to build up to the actual movement,teaching the brain that those movements do not need to evoke pain. Taking away the pain and teaching you that chronic pain isn’t something to be worried about builds confidence and tackles catastrophizing. This study found that in the long term about GMI, a patient with chronic pain displayed, “minimal to no catastrophizing and fear avoidance behaviors.”
- Graded exposure therapy
Graded exposure therapy tackles negative perceptions and fears about pain in a gradual yet head on way, aiding patients to face the activities that they fear a step at a time to remove the fear. Graded exposure has had some success in treating pain catastrophizing as explained here.
- Interdisciplinary rehabilitation programmes
One of the most successful treatments for pain catastrophizing is a combination of CBT techniques and physical therapy to build up the body’s fitness and range of motion. CBT techniques when combined with a physical aspect to teach the patient how to move their body in a safe way, not only can build confidence but can really tackle fear and worry from both angles. This type of treatment has shown to produce positive results as shown here.
With the right treatment and guidance, pain catastrophizing can be overcome; your pain does not have to control your life!
References
- Pain Medicine, Volume 17, Issue 11, Pages 2026–2035, Julia R. Craner, PhD, Jeannie A. Sperry, PhD, Michele M. Evans, APRN, CNS, (2016), “The Relationship Between Pain Catastrophizing and Outcomes of a 3-Week Comprehensive Pain Rehabilitation Program”
- Phillip J Quartana, PhD, Claudia M Campbell, PhD, Robert R Edwards, PhD, (2009), “Pain catastrophizing: a critical review”
- Experimental Brain Research, Weissman-Fogel, Sprecher E, Pud D., (2008), “Effects of catastrophizing on pain perception and pain modulation.”
- Indian Journal of Psychological Medicine, Lawrence Leung, (2012), “Pain Catastrophizing: An Updated Review”
- Practical Pain Management, Volume 15, Issue 6, Robert J. Gatchel, PhD, ABPP and Randy Neblett, MA, LPC, BCB, (2017), “Pain Catastrophizing: What Clinicians Need to Know”
- International Review of Neurobiology, Volume 139, Pages 129-157, Beth D.Darnall, Luana Colloca (2018), “Chapter Six – Optimizing Placebo and Minimizing Nocebo to Reduce Pain, Catastrophizing, and Opioid Use: A Review of the Science and an Evidence-Informed Clinical Toolkit”
- Andrea Burri Soshiro Ogata, David Rice, Frances Williams, (2018), “Pain catastrophizing, neuroticism, fear of pain, and anxiety: Defining the genetic and environmental factors in a sample of female twins”
- PAIN Reports, Volume 2, Issue 5, p e617, Chehadi, Omara; Suchan, Borisb; Konietzny, Kerstina, et al (2017), “Gray matter alteration associated with pain catastrophizing in patients 6 months after lumbar disk surgery: a voxel-based morphometry study”
- Physiotherapy Theory and Practice, Shepherd M PT, DPT, OCS, FAAOMPT, Louw A PT, PhD, Podolak J PT, DPT, (2018), “The clinical application of pain neuroscience, graded motor imagery, and graded activity with complex regional pain syndrome-A case report.”
- Beth D. Darnall, John A. Sturgeon, Karon F. Cook, et al, (2017), “Development and Validation of a Daily Pain Catastrophizing Scale”
Please note: This article is made available for educational purposes only, not to provide personal medical advice.
Pathways Helps You Break The Pain/Fear Cycle
Enjoy any one of our hundreds of meditations